加科思利用诱导变构药物发现平台,自主研发了SHP2抑制剂JAB-3312,目前在中美两国进行临床研究,并均在美国获得FDA用于食道癌(包括食管鳞癌)的孤儿药认定。 加科思的SHP2抑制剂是全球第二个获得美国FDA批准进入临床开发的同类项目。
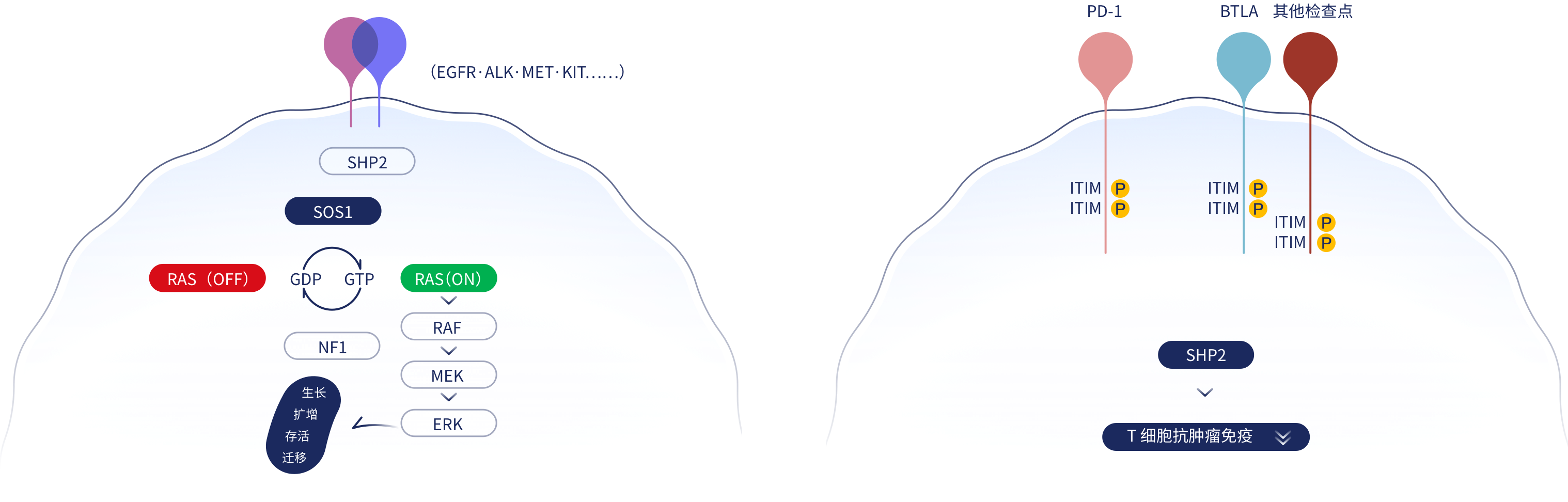
SHP2,也称为PTPN11,是一种磷酸酶,能够对底物蛋白去磷酸化,是调控细胞功能的重要分子。在RTK通路中,SHP2位于RAS上游,介导肿瘤增殖; 同时SHP2位于免疫检查点PD-1的下游,抑制T细胞抗肿瘤作用;还处在CSF-1R下游,促进肿瘤相关巨噬细胞功能。因此,靶向SHP2可起到多重抗肿瘤作用。
|
药物 |
联合用药搭档 |
地区 |
试验阶段 |
适应症 |
登记信息 |
|
|---|---|---|---|---|---|---|
|
JAB-3312 |
戈来雷塞 (KRAS G12Ci) |
中国 | IIa期 | 晚期实体瘤 |
ClinicalTrials: NCT05288205 CDE Number: CTR20220587 |
|
| Sotorasib (KRAS G12Ci) | 全球 |
I/IIa期 |
晚期实体瘤 |
ClinicalTrials: NCT04720976 CDE Number: CTR20212254 |
||
| 奥希替尼(EGFRi) | ||||||
| 帕博利珠单抗 (PD-1 mAb) | ||||||